The impact of meditation aided by VR technology as an emerging therapeutic to ease cancer related anxiety, stress, and fatigue
- 1College of Computing and Software Engineering, Kennesaw State University, Kennesaw, GA, United States
- 2PNI Therapeutics, New York, NY, United States
- 3Cancer Doctor, LLC, Kennesaw, GA, United States
- 4Northeastern University, Boston, MA, United States
Patients diagnosed with cancer experience a high degree of stress as well as side effects from treatments that can greatly impact their quality of life. Many patients experience long-term side effects such as pain, fatigue, anxiety, depression, and cognitive dysfunction. Several studies have reported that the use of virtual reality (VR) interventions show substantial benefits in reducing symptoms of anxiety, depression, pain, and cognitive functions in cancer patients undergoing therapy. In this study we analyzed the acceptability, feasibility, and tolerance of PNI Thrive, a 10-min VR guided meditation application, as an adjuvant digital therapeutic aid for cancer patients in a clinical setting. Patients diagnosed with various cancers, and at different stages of therapy, participated in this study. Our data suggests that the adjuvant VR treatment was successful in making patients feel calmer, more relaxed, refreshed, and more empowered. We propose that routine exposure of patients to VR interventions will help improve their response to anti-cancer therapies and quality of life.
1 Introduction
People feel a range of emotions when confronted with a diagnosis of cancer. Their life has been disrupted suddenly by an unwelcome event. Patients experience a tsunami of information from their doctors regarding their diagnosis, lab work, and treatments. There is a high degree of uncertainty about their future, and many experience stress, anxiety and depression. Negative emotions influence mental and physical health and result in diminished quality of life and sub-optimal treatment and health outcomes (Conley et al., 2016).
In order to cope with their disease, patients use various reward and empowerment strategies to make them feel better both physically and psychologically (Zion and Crum, 2018). One emerging area within Complementary Alternative Medicine (CAM) is Complementary Integrative Therapies (CITs) (Maindet et al., 2019). CITs, specifically mind-body therapies such as yoga and meditation, have been shown to be efficacious in helping cancer patients manage stress (Glaser et al., 2000). Recent studies have explored the use of virtual reality (VR) simulations using CITs to reduce stress, lessen anxiety, improve overall healing, and increase the efficacy of traditional standard of care treatments in a variety of health areas. A recent systematic review showed that multiple VR studies reported significant improvements in anxiety- and depression-related measures (Kemp and Botella, 2019). Studies assessing the use of VR interventions have shown significant effects on reducing symptoms of anxiety, depression, pain, and cognitive function in cancer patients (Ahmad et al., 2022). Overall, patients that are less stressed, have a positive attitude, and participate in self-care, have better health outcomes.
VR as a complement to standard of cancer care and/or alternative cancer treatments provides cancer patients with an affordable, accessible, engaging therapeutic intervention that has little to no side-effects and that can improve the quality of their life (Serra et al., 2012; Andrea et al., 2015; Chirico et al., 2020).
In the current study, the acceptability, feasibility, and tolerance of the use of a 10-min VR guided meditation application, PNI Thrive, was used in a clinical setting at Immunity Therapy Center (ITC).
Specifically, the study aimed to.
1. Observe the most relevant patient population, and patients’ willingness to use VR treatment.
2. Determine the objections to use of VR such as skepticism, not wanting to use technology, psychological considerations.
3. Gather measurements of patient reported outcomes regarding levels of: anxiety, relaxation, fatigue, empowerment, and other self-reported measures of overall mental and physical wellness pre- and post-VR application.
4. Identify the obstacles to incorporate VR treatment into the flow of usual care including management of hardware, software, patient education regarding use of VR treatments.
5. Ascertain the prevalence, if any, of patient reported adverse effects including ill-fitting hardware, eye-strain, nausea, and anxiety.
2 Methodology
2.1 Participants
Thirty-six patients diagnosed with various cancers, at different stages were included in the study (n = 36). Two patients did not report some information, so they are excluded from the demographic information as it was null. Patients who were treated at Immunity Therapy Center (ITC) from July-October 2021 were provided an information sheet with an introduction from Dr. Carlos Bautista, Medical Director of ITC. The information sheet told patients that ITC was conducting a Virtual Reality clinical research study and invited them to participate on a voluntary, non-paid basis. Participants who wanted to participate provided informed, written consent. Participants were requested to use the VR treatment for 5–10 days and were told they could opt out of the study at any time for any reason.
2.2 Immunity Therapy Center
Patients undergoing treatment at Immunity Therapy Center (ITC) were provided the VR experience and ITC was responsible for conducting and collecting the surveys used in this study.
ITC is an inpatient and outpatient integrative cancer treatment center located in Tijuana, MX, consisting of a team of medical doctors led by Medical Director Carlos Bautista, MD, who has over 25 years of experience in treating cancer patients.
The center receives patients from around the world. Approximately 90% of the patients arrive from the United States having already received the standard of care for various cancers. Dr. Bautista is onsite meeting with patients daily Monday-Friday. Patients arriving at ITC are seeking a form of comprehensive alternative and complementary care to improve their quality of life in hopes of improving long term outcomes.
All patients receive a treatment plan approved by Dr. Bautista for their condition. Approximately 80% of treatment plans are identical between all patients with the remaining 20% tailored for the patient’s specific type and stage of cancer. Treatment plans include the items listed in the addendum.
Patients undergo routine weekly blood lab work and imaging as needed and meet with their assigned MD a minimum of 4 days per week. Dr. Bautista meets with the patients a minimum of 1 day a week. The medical team meets daily to evaluate all patient cases. Patient treatment plans are adjusted as needed after a thorough clinical review of each patient’s response to their assigned treatment plan. The treatment plans at ITC are for a minimum of 4 weeks and are extended upon joint agreement between the patient and MD.
2.3 Participant exclusions
Patients with certain pre-existing medical conditions based on general safety recommendations for VR headsets such as: patients with epilepsy, seizures, seizure risk, sensitivity to flashing lights, motion sickness, etc., were excluded from participating in the study.
In addition, the following patients were excluded.
1. Non-consentable patients (such as patients who are unable to provide informed consent or patients under legal guardianship).
2. Patients under the age of 18.
3. Patients with objections to virtual reality, use of wireless devices, etc.
4. Patients with a current eye infection.
5. Pregnant patients.
6. Patients admitted as an emergency.
7. Patients participating in another clinical study that may have a potential impact on the endpoints of this study.
8. Patients with a medical history of dementia, schizophrenia, hallucinations, panic attacks and epileptic seizures.
9. Patients who carry a pacemaker or defibrillator device.
10. Patients with brain tumors.
11. Patients taking neuroleptic or anti-epileptic drugs.
12. Patients with active alcohol and/or substance abuse.
2.4 Study design and procedure
Participants were randomly assigned to Group 1 (m = 9), where the VR treatment was the first treatment the patient would receive that day, or to Group 2 (n = 25), where the VR treatment was the last treatment the patient would receive that day. All VR treatments were performed under direct supervision of ITC staff. Participants were provided and fitted with a Meta Quest 2 VR headset (Meta, 1 Hacker Way, Menlo Park, CA) along with two controllers. Patients receiving the VR treatment were in a seated or prone position. Participants navigated through the 10-min VR experience with the controllers and their gaze. The virtual content consisted of:
1. An outer space environment with a representation of an asteroid, stars and the Sun.
2. A deep breathing exercise.
3. A medical illustration segment that included a representation of T-cells where participants could direct them with their gaze to destroy a representation of cancerous cells.
4. A closing segment that included a mandala (Secular version) or the Star of Bethlehem (Christian version).
In addition to the virtual visual content, the VR treatment included ethereal background music and a male voice over for the guided meditation. The voice over is currently in English, but is easily modifiable to other languages. At the start of each VR treatment participants were given the choice of a Secular voice-over or a Christian voice-over. The Secular voice-over referenced the healing power of the Sun and the Universe, whereas the Christian voice-over referenced the healing power of God (e.g., invoking the name of The Lord Jesus). There were ten participants who chose at least 50% of their sessions in the Secular format (m = 10) while twenty-six chose the Christian format (n = 28). Participants could choose their format for each session, so many chose to at least sample both formats. There were a total of 54 secular sessions (m = 54) and 157 Christian sessions (n = 157).
Participants were assigned a patient number to ensure privacy and so that all data were anonymized. Prior to the first time use of the VR treatment, ITC staff recorded patient gender, age, and education. Patients were given a self-administered questionnaire that primarily focused on quality of life questions which they completed prior (pre-VR) to the VR treatment and then after (post-VR) the VR treatment. Additionally, ITC staff took patients’ blood pressure readings prior to the completion of the pre-VR questions and then again prior to the completion of the post-VR questions.
The surveys, patient interactions, patient participation, and the overall procedures for the study were governed by the ITC Board of Ethics and overseen by their qualifying physicians. This Board of Ethics reviewed the study, the procedures, and the patient selection and handling procedures to make sure that everything was in compliance with and governed by their ethical oath. The Board of Ethics formation and accreditation document is attached at the end of the article.
2.5 Patient groups
The patients were divided into two sets randomly, one control group (m = 18) and one test group (n = 36). The control group received all of the same treatments and distribution of treatments as the test group. The two groups were constituted in a manner that made the VR treatment the only variable of change. The control group was demographically similar to the test group as well. This testing scenario was designed to ensure equity across the participants.
2.6 Patients’ clinical characteristics
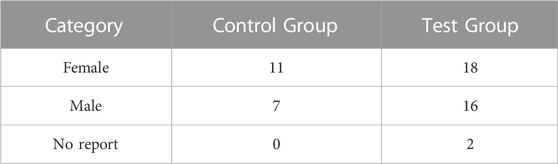
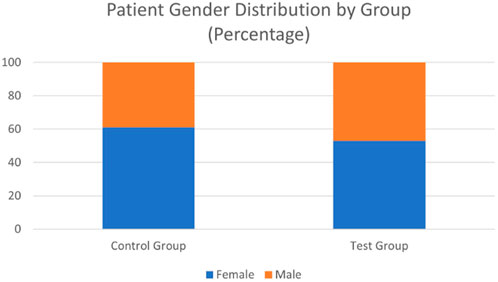
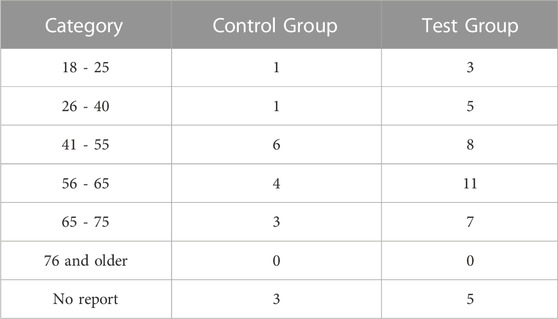
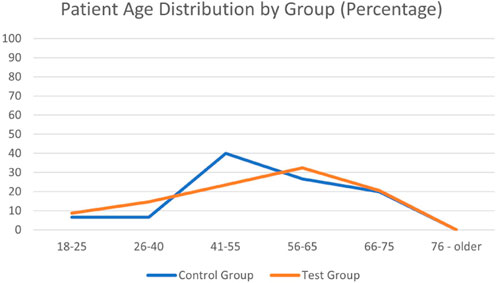
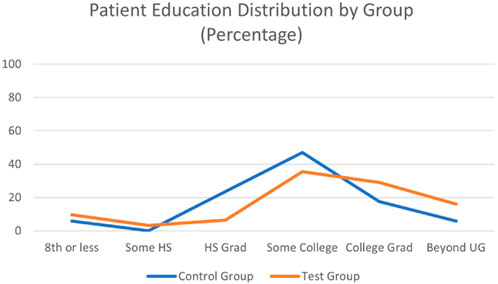
Patients’ clinical characteristics including type of cancer, and current medications were obtained from ITC medical charts. Demographically, there was an even distribution across genders (Table 1; Figure 1), uniform distribution across the age ranges (Table 2; Figure 2), and an education distribution that slightly favored those who at least graduated high school (Table 3; Figure 3). Of the 18 control participants, only 3 did not share complete demographic info. Of the 36 test participants, only 2 did not share any demographic information. The control group improvements and overall health improvements for them are analyzed in Section 3.6.
2.7 Data analysis method
To assess the effect of the VR application on patient-reported outcomes, paired t-test was performed. Paired t-test is a statistical procedure used to determine whether the mean difference between two sets of observations is zero (Statistics Solutions, 2021). In a paired t-test, each parameter is measured twice, resulting in pairs of observations. In this study, two sets of data were pre-VR and post-VR patient-reported outcomes. In paired t-test, there are two hypotheses; the null hypothesis that assumes the true mean difference between two sets is equal to zero, and the alternative hypothesis that assumes the mean difference is not zero. The decision to accept or reject the null hypothesis is determined by the p-value. If the p-value from the test is less than 0.05, we reject the null hypothesis and accept the alternative hypothesis, concluding that the difference between the two sets is statistically significant. On the other hand, if the p-value is greater than 0.05, we accept the null hypothesis concluding that the difference between the two sets is not statistically significant.
2.8 Statistical significance
The p-values were obtained for every single paired-tests. Since all the values were less than 0.05, the magnitude of improvement in each group for each Patient Reported Outcome (PRO) is statistically significant. To ensure that the statistical significance carried through to our reported outcomes we analyzed only the patient’s data as compared with their own data, not with the group as a whole. This isolated the effect of the variability with scaled qualitative data by avoiding direct comparison from patient to patient (i.e., we took the delta (differential) pre- and post-treatment for that patient only and then used that delta across the patient set for averages).
3 Results
3.1 Overall test group
The results show a significant and noteworthy increase of PROs of mental and physical health post-VR treatment vs the pre-VR treament for the test group (those using the guided VR therapy) (Smyth and Arigo, 2009). To validate this, we concern ourselves with two major concepts. First, we will examine the delta between the pre- and post-treatment surveys. As indicated above, each patient was asked to assess and report their feelings about their condition, their health, and their outlook by responding to a survey questionnaire. With all other factors being fixed, the sole differential is the VR guided therapy, so we assert all effects of the post-treatment survey to be fully dependent on this factor. For disclosure, we understand that each patient is different and that their conditions vary, but with the diversity of patients being treated and with us only comparing their own post-treatment PROs to their pre-treatment PROs, we have isolated the treatment’s effects. Second, we will look at the comparison from the control group (those who did not participate in the VR treatments) with the test group to note the effects of the VR treatment compared to non-treatment.
We will first consider the questionnaire itself on a question by question basis. The questionnaire is attached in the addendum. The first section gathers the basic demographic information of the patient, followed by questions pertaining to learn about their prior experience(s) with virtual reality in the second section. The third section is the beginning of testable questions to determine PROs before each treatment session. This is very similar to the fourth section, the post-test, and offers the delta (differential) for our initial results. Section 4 also includes questions about the VR aspects in particular, but these questions will be addressed later in this discussion. The final section, Section 5, asks about the patient’s views on recommending VR therapy to others and asks if their views on mind-based healing have changed in any way.
For our initial determinations we compared the deltas from Section 3 to Section 4 where the same questions were asked pre- and post-treatment. Each question is asked on a scale where each response is given a value score. With five total responses each score is from 1 to 5 based on the selection. For example, the top response, ‘Very Good’, is given a 5. Similarly, the lowest response, ‘Very Bad’, is given a 1. We averaged the responses of all individuals within the group for this initial analysis.
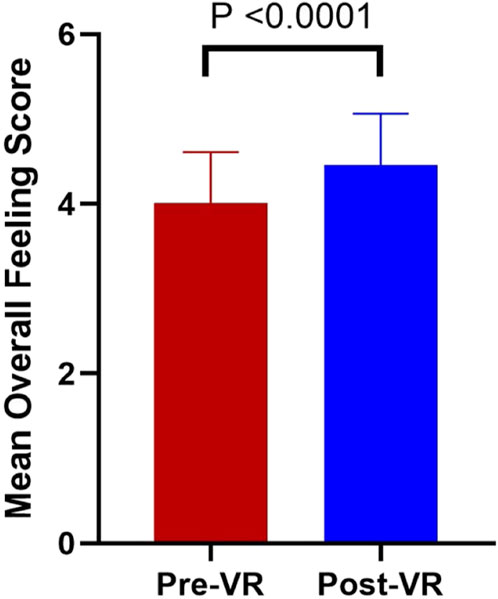
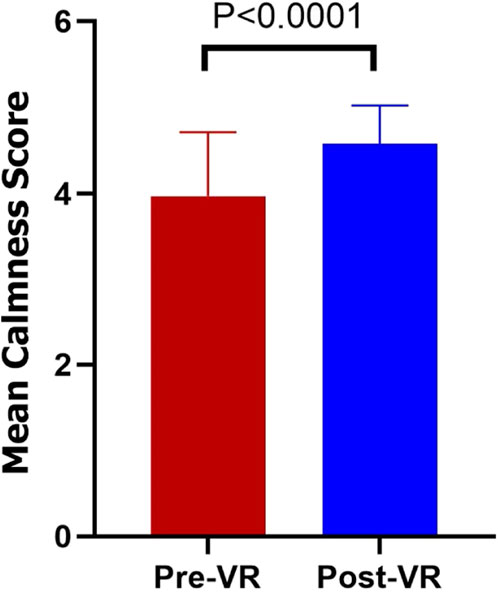
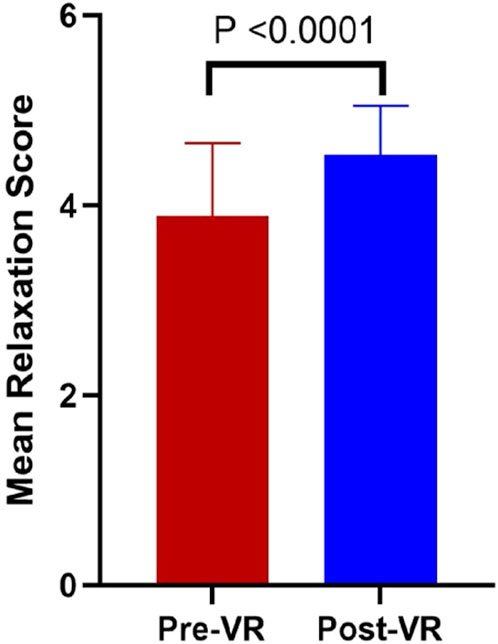
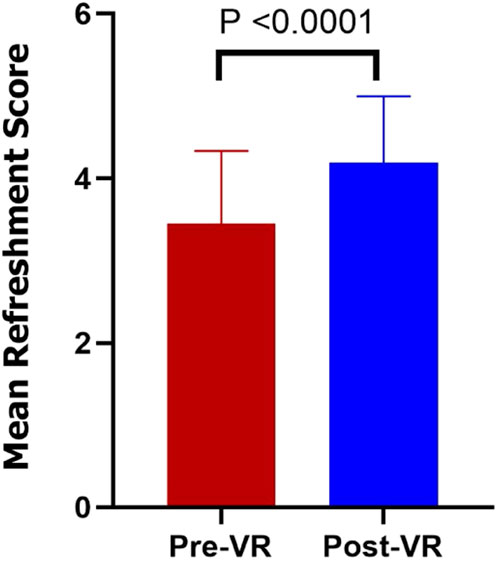
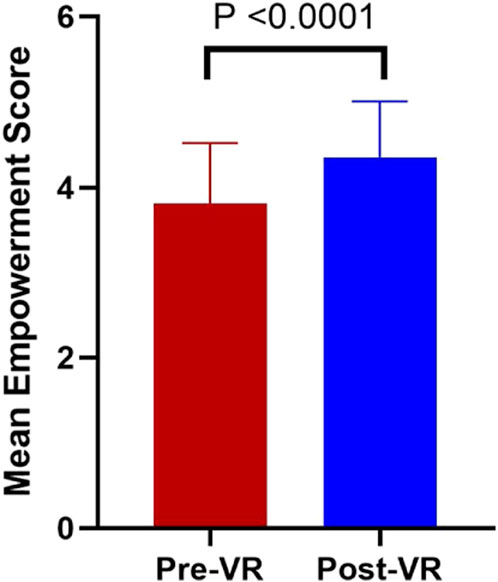
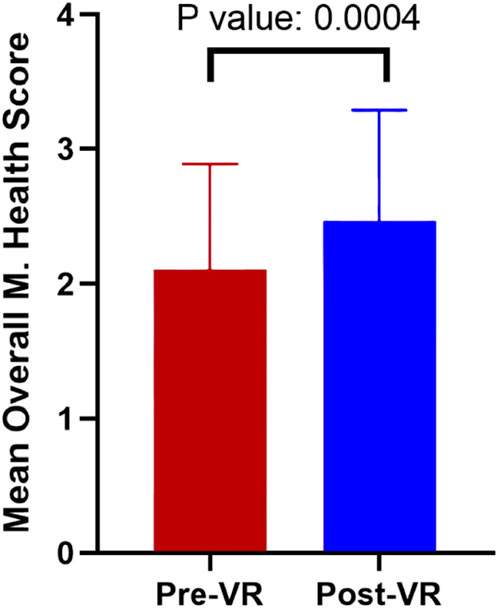
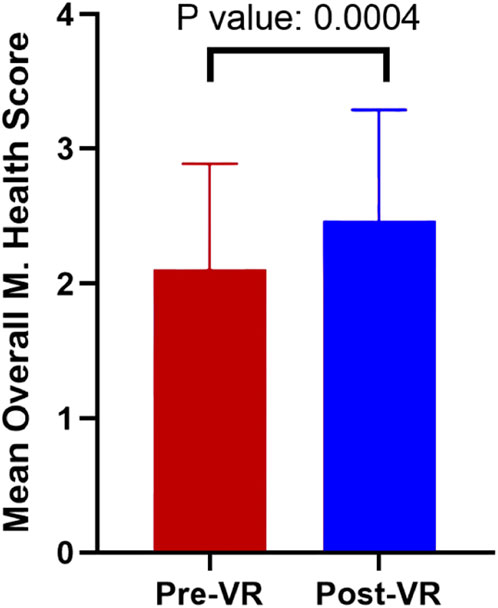
The treatment group, those who utilized the VR guided therapy, showed an improvement of 0.454, or an 11.35% increase in their overall feeling in response to a question about how they feel right now (Figure 4). For this graph, and all others with bars, the bars show the standard deviation. The following questions deal with the specific feelings of the patient. The second question is about the patient’s sense of calm. The test patients showed an improvement of 0.605, or 15.1% (Figure 5). The next question concerns their relaxation. The patients reported an improvement of 0.651, a 16.3% improvement (Figure 6) after the use of the VR treatment. The fourth question asks the patients about their level of fatigue vs their level of refreshment. The test patients responded with an improvement in their level of refreshment of 0.686, nearly 17.2% (Figure 7). The fifth rates their feeling of empowerment. The test group showed an improvement of 0.488, or a 12.2% increase in their feeling of empowerment (Figure 8). The final two questions of comparison ask overall feelings of health. Question 6 is about overall health, and among those that engaged in the guided VR therapy there was an overall movement towards excellence of 0.411 (10.3%) (Figure 9). Question 7 asks about mental and emotional health. Those in the test group showed solid progress towards improved mental and emotional health of 0.397 (9.9%) (Figure 10). As can be seen from these questions, there was a strong qualitative improvement across the patients who utilized the guided VR therapy in their treatment regimen.
To expand on each of these we examine each one statistically.
The process of gathering the data that is represented in these figures is important for the validation of the results (Brownstein et al., 2018; Mcleod, 2021). To prepare the data we first eliminated the missing data sets (questions that were partially answered or not answered) which removed less than 4% of our sets. Next we found the average of the Patient Reported Outcomes (PROs). To group the data for the efficacy measurements we then divided the data into two sets, one set with patients who received four or fewer VR guided therapy sessions and another set who received five or more VR guided therapy sessions. The sets of data were then sorted into seven subsets based on PROs to run the paired t-test for each subset. For each subset two paired t-test were performed (for example, Q3.1 and Q4.1 Overall Feeling). Finally, we found the difference between the post-VR average value and the pre-VR average value to calculate the magnitude of improvement in PROs.
3.2 Effect of number of treatments
The results were then tabulated (Table 4) to compare the effects of numbers of treatments on PROs scores. As previously discussed, the overall average improvement from the pre-VR to post-VR PROs is significant; however, there is increasing interest when we look at the breakdown by the number of treatments. Looking at them one by one, we start with the first pair, Q3.1 and Q4.1 (Overall Feeling Right Now). Patients’ health with four or fewer VR guided therapy sessions improved by 0.42 quality points, or a 10.8% improvement and those with five or more sessions improved by 0.51 quality points, or a 12.2% improvement. This suggests that patients who had more VR sessions improved at a higher rate (around 1.4% more) than those with fewer sessions. It should be noted that patients with only one VR guided therapy session still improved their outcomes, but the more treatments patients receive the greater the improvement.
The second question, related to levels of anxiety, Q3.2 vs Q4.2, also showed significant improvement. The overall improvement for patients with four or fewer treatments was 0.45 quality points, or over an 11% improvement, whereas those patients with five or more treatments improved 0.72 quality points (an 18.8% increase), so over 7.8% better. The data show that the increased visits help patients feel calmer. The third pair, Q3.3 and Q4.3 (Tensed or Relaxed), shows the same pattern of improvement with an increase of 0.59 quality points, over 14.8% with those receiving 4 or fewer treatments, but over 0.75 quality points (or over 20%) increase with those receiving 5 or more treatments (this is nearly a 6% growth). This suggests that increasing the amount of time the patients have with the VR guided meditation therapy helps them feel more relaxed. The fourth question pair, Q3.4 and Q4.4 (Fatigued or Refreshed), shows a slightly different trend. In analyzing the improvement we see the growth of 0.82 quality points (a 24.64% increase) with those having four or fewer, but those with five or more treatments were over 4% less. The fifth question pair, Q3.5 and Q4.5 (Dispirited vs Empowered), seeks to analyze the effect of increased treatments on the patient feeling empowered. This pair showed an improvement of 0.58 quality points (15.6% increase) with four or fewer treatments, but slightly less improvement with the increased number of treatments (about 4.8%). The final two pairs ask about overall and general health. Q3.6 and Q4.6 seek to assess overall health from poor to excellent. The patients that had four or fewer treatments showed an increase of 0.44 quality points (over 15%), but those users who had five or more treatments increased by 16.8%, indicating an increasing feeling of overall excellent health. Q3.7 and Q4.7 asked the overall feelings about emotional and mental health. The increase in sessions for each patient yielded an improvement of 0.31 (a 12.4% increase) for those with four or fewer treatments, but 0.44 quality points (an 18.8% increase, over 6% better than those with fewer treatments) for those with over five visits.
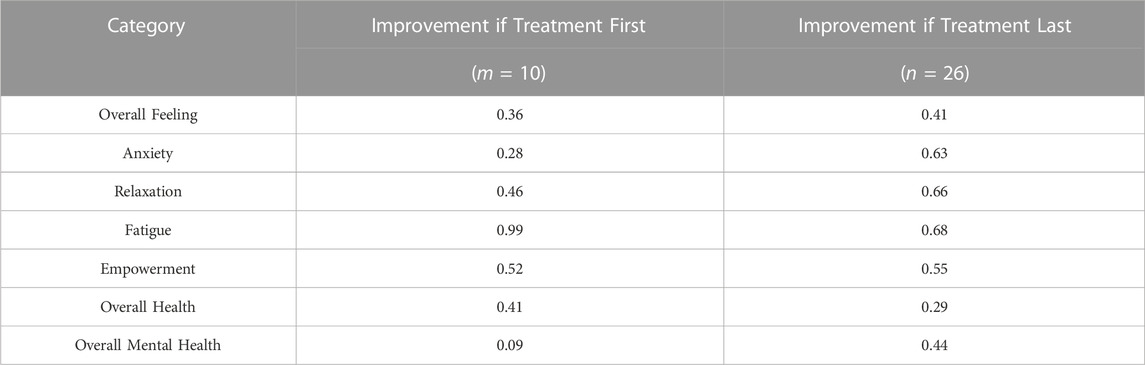
3.3 Effect of treatment schedule
Upon enrollment, participants were randomly assigned to either Group 1 or Group 2 (Brownstein et al., 2018). Participants in Group 1 (m = 10) received VR treatment as their first treatment of the day whereas participants in Group 2 (n = 26) received VR treatment as their last treatment of the day. This assignment was recorded in Q1.4 in the survey questionnaire. The analytical method used to assess whether there are any differences in the two groups was similar to the analysis discussed above. Both groups, whether having VR guided meditation first or last with respect to their other treatments, showed similar improvement. Those doing their VR meditation first improved on average by 0.443 quality points, or over 11.7%. Those ending their treatment schedule with the VR meditation improved on average by 0.521 quality points (over 13%). While the overall improvement was noteworthy for both groups separately, the experimental group’s responses to the PROs varied (i.e., some were better for the first group, others for the second group). As shown in Table 5, the responses varied for each group. The five PROs show improvement for those doing their VR guided meditation at the end of treatments vs those having the VR treatment first. Contrariwise, there are two PROs, Fatigue and perceived Overall Health, where those having the VR treatment first showed more improvement than those having the treatment last.
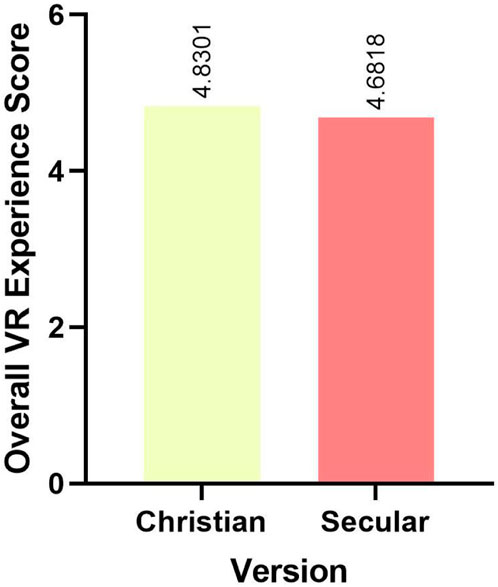
3.4 VR guided meditation voice over
At the start of each VR treatment, participants were given the choice of a Secular voice-over or a Christian voice-over. The Secular version referenced the healing power of the Sun and the Universe, whereas the Christian version referenced the healing power of the Lord and God. Patients were asked to select the version of the VR for the day, and their answers were recorded as 1 if they viewed the Christian version or 2 if they viewed the Secular version. To compare if there are any differences in the Secular or the Christian version of the application, we assessed the patient’s overall VR experience. The rating was as follows.
• Disliked it a great deal: Value of 1
• Disliked it somewhat: Value of 2
• Neither liked nor disliked it: Value of 3
• Liked it somewhat: Value of 4
• Liked it a great deal: Value of 5
The average score of the overall VR experience for patients who viewed the Christian version was 4.83 while the average score of the overall VR experience for patients who viewed the Secular version was 4.68 (a significant difference with a p-value less than 0.05). Thus, the Christian version of VR offered a better VR experience for patients than the Secular version (see Figure 11). As noted in the demographics section, there were a number of patients that used one version predominantly or completely, but there were two that were nearly equally split across the versions, so 1 credit to each, thus the total of (n = 38).
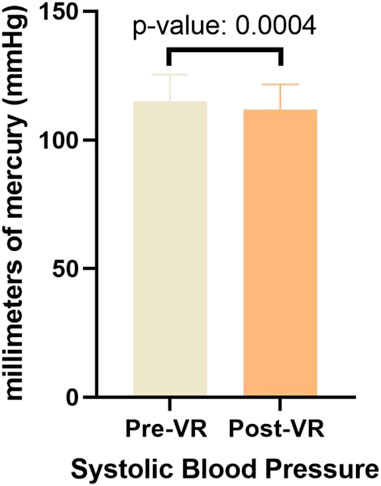
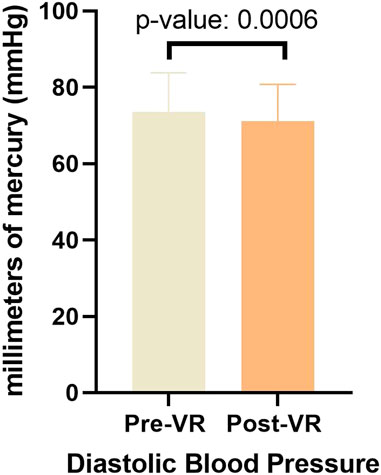
3.5 Effect on blood pressure
Paired t-test was performed to evaluate whether there is a difference in the blood pressure before and after VR therapy (US Department of Health and Human Services, 2021). Two paired t-tests were performed; one for the systolic blood pressure and another for the diastolic blood pressure. As Figures 12 and 13 shows, a statistically significant decrease in both systolic and diastolic blood pressure was observed after VR treatment (p-value ≤0.05). The average systolic blood pressure change from pre- to post-treatment measurement was a reduction of 3.66 (i.e., for each pair of measurements we calculated the delta and averaged those deltas). The average diastolic blood pressure average delta change was a reduction of 1.94. While n = 36, there were a total of 140 measurement pairs. A decrease in systolic blood pressure, especially, has meaningful medical benefits.
3.6 Overall control group
To remove the inherent bias of using only data from the VR test group we gathered data from a control group. As shown in Section 2.6, the control group was drawn from the same population as the test group (thus they share primary characteristics and match demographically). The control group received treatments from the same pool of treatments as the test group with each set of treatments being drawn from the same distribution of treatments. Statistically there is no difference from the control group with the test group (the only difference in the two groups being the inclusion or exclusion of the VR guided therapy). The first series of questions assessed the groups overall feelings about their health and mental state. Comparing the control group to the test group, we see that their initial assessment varied by only 2.22% (σ of 0.39). Initial assessment is an aggregate score of mental health based on the first seven questions of the survey (as listed above and shown in the attached document). This shows the alignment of the groups and clarifies the exclusion of the VR guided therapy. By performing a cross-validation of the data set we can see that with a p-value of 0.03 shows that the populations were equal in makeup and distribution. It was vital to the study that we were able to isolate the effect of the VR guided therapy and this data proves that we were successful. Further, to isolate the effect of the VR guided therapy we can see that the control group improved through treatment alone at about 5.6%, where the test group that added the VR guided therapy improved from 9.9% to 17.2% (or, on average, about 13.19%).
4 Discussion
The data and experimentation show the valuable effect of utilizing VR guided meditation alongside standard and alternative cancer treatments to improve PROs of mental and physical health. Each qualitative category showed increasing efficacy and better outcomes for the patients that used the VR guided therapy, as detailed above. We can look at each of these outcomes in summary below.
First, the control group showed two valuable insights. It was imperative, and it was shown, that the control group (those who did not receive the VR guided meditation) was made up of a similar population as the experimental group (those that did receive the VR guided meditation). There was no difference in their overall treatment plans (in aggregation they all received the same kinds of treatments from the same pool of available treatments with similar distribution of treatments in both pools of patients) other than the control variable of VR guided meditation. Additionally, we have shown that the experimental group showed marked improvement over the control group by over 13% on average. This first insight offers demonstrable evidence of the powerful influence of VR guided meditation as an effective addition to cancer treatment. Thus, the net effect of the VR guided therapy is demonstrably positive above the baseline improvement from therapy alone.
Second, the experimental group showed a strong generalized improvement along with significant improvement in each area of study. The general improvement showed, on average, that the patients improved in their PROs on average by over 15% (ranging from 9.9% to 17.2%). This finding was bolstered by the evidence that each qualitative category showed improvement, a strong result for the experimental group. We next examined the experimental group by the number of VR guided meditation treatments that they received. The evidence showed that even one VR guided meditation treatment showed immediate improvement and, importantly, that the more VR guided meditation sessions the patients received the better their outcomes (Kiecolt-Glaser et al., 2002; Garland et al., 2021). The next division was based on the schedule of the VR guided meditation. The experimental group was divided into those who received their VR guided meditation first (before their other treatments) and those who received it last (after their other treatments). Overall, both groups showed improvement without respect to the timing of their treatment, but those receiving their treatment last showed the most overall improvement (total average improvement across all categories viewed in aggregation). There were some reasonable findings that some patients felt more fatigued when having the VR treatment as the last treatment of the day, but the feelings were very similar for the control group (meaning that the day of treatment was grueling and fatiguing, but not necessarily indicative of any specific one of the treatments). We cannot deny that fatigue is a factor by the end of the treatment schedule, but our goal was to show improvement occurred regardless of timing, though it proved more effective as the last treatment of the day. It was an important finding that this proposed treatment fits into the regimen of treatments available without significant disruption, but offers increased quality of outcome for the patients. Additionally, there were findings that the alignment of the voice-over for the VR guided meditation with the patients’ preferences showed a stronger improvement in efficacy. For clarity, while the patients were not directly asked their religious preferences, they were told to indicate this in their choice of voice-over. However, we wanted the patients to have a choice, so they were able to select either voice-over, and did so as indicated in the session data vs. the patient summary data in the data analysis. There were many patients, approximately 80%, that tried both voice-over options at least once. While there were 2 patients that used both fairly equally, the predominance favored heavily their aligned preference. Based on this affinity, and the patients’ comments, it appears that the more the patient connects with the intent of the voice-over the stronger their connection to the treatment and thus the greater improvement in their overall health feelings and PROs, though this further inference should be tested more completely in future work. As stated, this was also relayed via patient comments in their post-treatment surveys. This finding is significant and will be part of the expanded future study. Finally, the data show quantitative improvement in the blood pressure of the patients. The calming effect of the VR guided meditation is demonstrated in the reduced blood pressure of patients after their treatments (by comparing the average improved blood pressure delta from the control group to the same for the test group). In fairness, there may be other items affecting this blood pressure outcome (such as rest, relaxation, pose, etc.) so this needs to be investigated more fully in future work. We look to expand this area of the research as well in the future as we are already seeing significant improvements from the treatment. The results of this study indicate that the patients had demonstrable overall improvement in their feelings about their emotional and mental health.
Overall, there were many relevant discussions for each section. In the case of fatigued vs. refreshed, the increase in treatments leads towards the patients feeling more refreshed up until a point, but then the effect begins to lessen (we can see this effect because we have pre- and post-treatment questionnaires from the patients and can track this effect and efficacy over time). We feel strongly that this is more a function of the patients using the same treatment visualization over and over rather than a loss of efficacy, a point which we will test in future work. With respect to the Dispirited vs. empowered discussion (and other areas where extended numbers of VR sessions were involved), the disparity in outcomes is likely due to a lack of variety in the programming, but this must be tested for certainty in future work. The efficacy is clear up to a certain point for all patients, but for some small portion of the patients, their improvements diminish over time. They still improve, but less so than some. With regards to the treatment schedule, the results (showing the increase in fatigue for those patients receiving VR treatment at the end of their day of other treatments) are not surprising considering the rigor of the treatment schedule (it is a full day of treatments). This means that patients are likely to feel more fatigued at the end of the day. Similarly, patients ending their day with the VR treatment are also exhausted from their treatments and thus feel slightly less improved in their overall mental health (though, as mentioned, they still improved significantly). Overall, these findings suggest that the timing of the VR guided meditation does not greatly impact efficacy as both timings showed strong improvement and every patient improved in every PRO in response to the treatment.
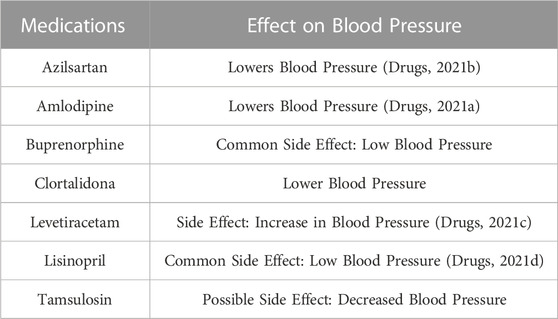
Finally, as a note for blood pressure effects, we add information from a related study. An NIH-funded study called the Systolic Blood Pressure Intervention Trial, also known as SPRINT, found that lowering systolic blood pressure in adults age 50 and older significantly reduced the risk of cardiovascular disease and death (U.S. Department of Health and Human Service). Other related studies also showed that lowering systolic blood pressure was associated with cognitive benefits. However, the effect of the patient’s current medication on blood pressure cannot be excluded. Based on the patient’s current medication history, there was a list of medications that had a potential effect on blood pressure (see Table 6). The effect of VR does have a positive effect in reducing blood pressure as per the statistical analysis. Nevertheless, the role of the patient’s concomitant and current treatment medication on these parameters cannot be excluded. Further information on the individual drug’s pharmacokinetics and the time interval between drug intake and patient exposure to VR needs to be explored.
5 Conclusion
The purpose of our study was to prove the positive impact of VR guided meditation on patients in cancer treatment. We were able to successfully isolate our primary variable, the effect of VR guided meditation, from the other variables through the use of our control group. We were able to show that the control group and the experimental group were nearly identically aligned in their entrance and exit evaluations sans the control variable. While all patients showed improvement from the treatments they were undertaking, those who added the VR guided meditation showed significant improvements over those patients in the control group. Further, we have shown that the effect on PROs is clear from the experimentation. Each area evaluated showed consistent improvement across the treatment schedule. The positive effects occurred with only one visit and continued to increase with the number of visits making it tenable that the more VR guided meditation the patients receive the better their outcomes. The positive effects occurred in PROs, positive overall health outcomes, and reduction in blood pressure. The positive outcomes have proven that the addition of VR guided meditation is worthy of inclusion in the overall treatment schedule for patients and that they can expect to see positive outcomes from this addition.
6 Future work
We will seek to improve on these excellent results with an expansion of the VR guided meditation. We have found several key conclusions that are worthy of expanded study such as the effect of treatment times, the effect of the treatments on blood pressure, and the increased efficacy of repeat treatments. The participants shared several suggestions that we will also take into consideration such as adding variety and selection to the VR guided meditations available to patients. We hope to expand the variety of meditations, voice-overs, and timings to better suit the patient’s preferences. We believe that the future work will show ever increasing impact of the positive effects of VR guided meditation.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of CBL Medical Clinic, S.C./Immunity Therapy Center. The patients/participants provided their written informed consent to participate in this study.
Author contributions
DF is the main author and editor of the paper; CS and RC contributed sectional paragraphs and supplementary material, YY, DA, SG, DV, SM, MeP, MaP, and NA created data analytics. All authors contributed to the article and approved the submitted version.
Acknowledgments
We thank Abhinav K. Jain, Department of Epigenetics and Molecular Carcinogenesis at the UT MD Anderson Cancer Center, Houston, TX, for helpful suggestions and contributions in developing the questionnaire, data interpretations, and editing this manuscript.
Conflict of interest
Author RC was employed by Cancer Doctor, LLC.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ahmad, S., Hekler, E. B., and Riva, G. (2022). Virtual reality for cancer patients: A systematic review and meta-analysis of clinical trials. Front. Psychol. 13 (1), 107–116.
Andrea, C., Lucidi, F., De Laurentiis, M., Carla, M., Alessandro, N., and Antonio, G. (2015). Virtual reality in health system: Beyond entertainment. a mini-review on the efficacy of vr during cancer treatment. J. Cell. Physiology 231 (1), 275–287. doi:10.1002/jcp.25117
Brownstein, D. J., Salagre, E., Köhler, C., Stubbs, B., Vian, J., Pereira, C., et al. (2018). Blockade of the angiotensin system improves mental health domain of quality of life: A meta-analysis of randomized clinical trials. Aust. N. Z. J. Psychiatry 52 (1), 24–38. doi:10.1177/0004867417721654
Chirico, A., Maiorano, P., Indovina, P., Milanese, C., Giordano, G. G., Alivernini, F., et al. (2020). Virtual reality and music therapy as distraction interventions to alleviate anxiety and improve mood states in breast cancer patients during chemotherapy. J. Cell. Physiology 1 (1), 5353–5362. doi:10.1002/jcp.29422
Conley, C. C., Bishop, B. T., and Andersen, B. L. (2016). Emotions and emotion regulation in breast cancer survivorship. J. Healthc. 4 (56), 56–22. doi:10.3390/healthcare4030056
Drugs (2021a). Drugs.com. Amlodipine: Drug uses, side effects & dosage. Available at: https://www.drugs.com/amlodipine.html (Accessed December 10, 2021).
Drugs (2021b). Drugs.com. Azilsartan medoxomil: Side effects, dosage & uses. Available at: https://www.drugs.com/azilsartan-medoxomil.html (Accessed December 10, 2021).
Drugs (2021c). Drugs.com. Levetiracetam side effects: Common, severe, long term. Available at: https://www.drugs.com/sfx/levetiracetam-side-effects.html (Accessed December 10, 2021).
Drugs (2021d). Drugs.com. Lisinopril uses, dosage, side effects & warnings. Available at: https://www.drugs.com/lisinopril.html (Accessed December 10, 2021).
Garland, S. N., Irwin, M. R., Posner, D., and Perlis, M. L. (2021). Are sleep continuity disturbance and fatigue prodromal symptoms of cancer development? Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6476185/ (Accessed December 10, 2021).
Glaser, R., Kiecolt-Glaser, J. K., and Malarkey, W. B. (2000). Stress, inflammation, and cancer: Evolving mechanistic and clinical models. Psychol. Bull. 126 (3), 363. doi:10.1146/annurev.psych.53.100901.1352
Kemp, A. S., and Botella, C., R. (2019). Virtual reality for anxiety and depression: A systematic review of clinical trials. J. Affect. Disord. 249 (1), 107–116.
Kiecolt-Glaser, J. K., McGuire, L., Robles, T. F., and Emotions, R. G. (2002). Emotions, morbidity, and mortality: New perspectives from psychoneuroimmunology. Annu. Rev. Psychol. 83 (53), 83–107. doi:10.1146/annurev.psych.53.100901.135217
Maindet, C., Burnod, A., Minello, C., George, B., Allano, G., and Lemaire, A. (2019). Strategies of complementary and integrative therapies in cancer-related pain-attaining exhaustive cancer pain management. Support. Care Cancer Official J. Multinatl. Assoc. Support. Care Cancer 27 (8), 3119–3132. doi:10.1007/s00520-019-04829-7
Mcleod, S. (2021). Value and statistical significance. Available at: https://www.simplypsychology.org/p-value.html (Accessed December 13, 2021).
Serra, D., Robertson Parris, C., Carper, E., Peter, H., Fleishman, S. B., Harrison, L. B., et al. (2012). Outcomes of guided imagery in patients receiving radiation therapy for breast cancer. Clin. J. Oncol. Nurs. 16 (6), 617–623.
Smyth, J. M., and Arigo, D. (2009). Recent evidence supports emotion-regulation interventions for improving health in at-risk and clinical populations. Curr. Opin. Psychiatry 22 (22), 205–210. doi:10.1097/yco.0b013e3283252d6d
Statistics Solutions (2021). Paired sample t-test. Available at: https://www.statisticssolutions.com/free-resources/directory-of-statistical-analyses/paired-sample-t-test/#::̃text=The%20paired%20sample%20t%2Dtest,r%esulting%20in%20pairs%20of%20observations (Accessed December 13, 2021).
US Department of Health and Human Services (2021). High blood pressure and older adults. Available at: https://www.nia.nih.gov/health/high-blood-pressure-and-older-adults (Accessed December 13, 2021).
Keywords: virtual reality, guided meditation, therapeutic, anxiety, stress, fatigue, guided therapy
Citation: Franklin DM, Silvestro C, Carrillo RA, Yang Y, Annadurai D, Ganesan S, Vasantham DSJ, Mettu S, Patel M, Patil MS and Akurathi ND (2023) The impact of meditation aided by VR technology as an emerging therapeutic to ease cancer related anxiety, stress, and fatigue. Front. Virtual Real. 4:1195196. doi: 10.3389/frvir.2023.1195196
Received: 28 March 2023; Accepted: 06 June 2023;
Published: 25 July 2023.
Edited by:
Michael J. Roy, Uniformed Services University, United StatesReviewed by:
Pinata H. Sessoms, Naval Health Research Center, United StatesKelsey Sprang Jones, Emory University, United States
Copyright © 2023 Franklin, Silvestro, Carrillo, Yang, Annadurai, Ganesan, Vasantham, Mettu, Patel, Patil and Akurathi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: D. Michael Franklin, mfranklin@trulyintegrated.com
 D. Michael Franklin
D. Michael Franklin Charles Silvestro
Charles Silvestro Robert A. Carrillo
Robert A. Carrillo Yewon Yang4
Yewon Yang4  Dharani Annadurai
Dharani Annadurai